Could this be the reason for the niacin study hype?
The new niacin study may have an underlying motive. Hmm, a new drug for Lp(a)?
Is There an Alternative Motive for the Recent Niacin Study?
I recently sent out a substack reviewing a recent niacin study in which the authors suggested that niacin is harmful and increases CVD risk.
New Niacin Study. Should we listen to it?
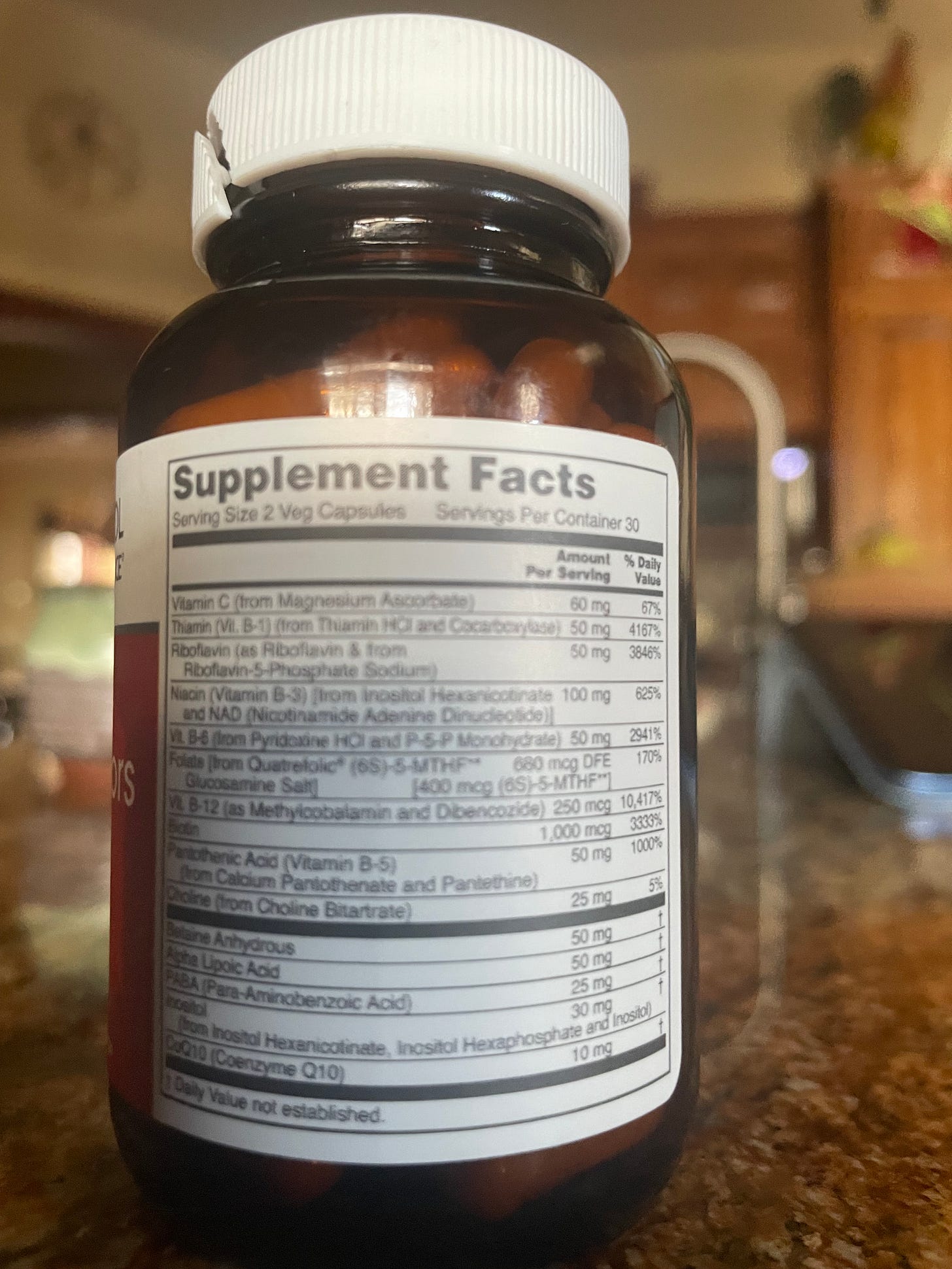
(On average, there is around 25 mg of niacin in a multivitamin/mineral supplement) Should We Listen to This New Study's Findings? A recent study came out suggesting that niacin supplementation is dangerous and increases CVD due to a newly discovered pathway.
I am a skeptic when it comes to medical professionals' claims that nutrients are harmful. As I stated in the previous post, we were left wondering what forms of niacin they examined.
Was it from whole foods, added to processed foods, or supplements?
What forms of niacin did they examine?
Was there any difference to nicotinic acid, nicotinamide, niacinamide, inositol haxanicotinate, NAD, slow-realease niacin or niacin that causes flushing?
We have no clue because they never provided this information.
According to the National Institute of Health, Niacin is Beneficial for CVD and Reducing Lipoprotein a.
(In bold is by me)
Very high doses of nicotinic acid—more than 100 times the RDA—taken for months or years are effective treatments for dyslipidemias. Nicotinamide does not have this effect because, unlike nicotinic acid, it does not bind to the receptors that mediate nicotinic acid’s effects on lipid profiles [1].
Studies conducted since the late 1950s show that these doses can increase high-density lipoprotein (HDL; good) cholesterol levels by 10%–30% and reduce low-density lipoprotein (LDL; bad) cholesterol levels by 10%–25%, triglyceride levels by 20%–50%, and lipoprotein(a) levels by 10%–30% [12]. Together, these changes in lipid parameters might be expected to reduce the risk of first-time or subsequent cardiac events, such as heart attacks and strokes, in adults with atherosclerotic cardiovascular disease.
However, despite dozens of published clinical trials, experts do not agree on the value of nicotinic acid to treat cardiovascular disease, especially given its side effects, safety concerns, and poor patient compliance [25].
In one large clinical trial from the 1970s, 8,341 participants age 30 to 64 years who had had one or more heart attacks were randomized to take one of five lipid-lowering medications, including 3,000 mg/day nicotinic acid, or a placebo for an average of 6.2 years [26]. Those taking nicotinic acid lowered their serum cholesterol levels by an average of 9.9% and triglyceride levels by 26.1% over 5 years of treatment.
Nine years after the study ended, participants who had taken the nicotinic acid experienced significantly fewer (11%) deaths from all causes than those who had taken the placebo [27,28].
What is Lipoprotein a (Lp(a)), and why don’t doctors test it?
Doctors never had a medication to treat elevated lp (a), so there was no reason for them to test for it since there was nothing in their toolkit to address it.
Medical professionals did not address this genetic CVD risk factor, even though the NIH has shown there are numerous studies indicating niacin therapy can reduce Lp(a).
Lp(a) is a form of LDL cholesterol that is “stickier” than other types, making it easier for the build-up to occur and arteries to become blocked.
A person’s genetic history and ethnicity determine their system's Lp(a) amount.
This Medical News Today article states:
About 20–25% of people around the world have a genetic version of ‘bad’ cholesterol called lipoprotein(a), or Lp(a) for short.
How can that be true when many doctors do not test for this marker? Do more people than we are aware of have this genetic CVD risk factor?
There is currently no cure or approved specific treatment for lowering Lp(a) levels.
By treatment, they mean no medication. Does that mean nothing exists to address this biomarker? Research indicates otherwise.
Researchers in Australia have now found a new potential oral medication developed to target Lp(a) can lower levels by up to 65%.
Ah hah, there it is!
They have now discovered a drug for Lp(a).
Granted, a 65% reduction is better than a 30% reduction via niacin. If they cared about CVD risk, they would have used niacin therapy in the past before a drug ever existed.
Instead, they did nothing! They didn’t test, and they did not use niacin therapy.
They go on to state:
Because Lp(a) is genetic, lifestyle changes like diet and exercise that may benefit other types of cholesterol do not help. There is currently no cure or approved specific treatment for lowering Lp(a) levels.
Again, none mention all the niacin studies that indicate a reduction in Lp(a).
Are they ignorant of niacin benefits or intentionally ignoring the research?
The New Drug
“Muvalaplin essentially blocks that binding from happening in the liver and therefore prevents the formation of Lp(a). It would provide an oral option for the treatment of patients with high Lp(a) levels to reduce their risk of heart disease.”
– Dr. Stephen Nicholls
The article concludes by stating that Lp(a) testing should be increased in those with CVD risk factors; however, (they state) there is not much a person can do since the new drug may still not be approved and available for another four years.
To me, this sounds a lot like C-19. The message was, “Not much you can do but wait for the new injection to save you.”
Bottom Line
Previous research indicated niacin is helpful for those with elevated Lp(a), a genetic CVD risk factor.
Doctors have not been testing for Lp(a) when they run a lipid panel because they do not have a drug to treat it.
A new drug to reduce Lp(a) will hit the market within several years.
Doctors state there is nothing you can do for Lp(a) but now encourage other doctors to test for this biomarker in their CVD-risk patients.
Patients will have to live with the fact that they have elevated Lp(a) and wait for the new drug to lower it.
UPDATE TO THIS POST (12/5/2024)
A recent Medscape article indicated that Eli Lily, who sponsored and designed the drug trials, is in phase II for their potential new drug to reduce genetic cholesterol determined by testing your Lp(a) levels. The drug is called muvalaplin.
The author of the Medscape article, Julie Steenhuysen, states that most people do not know they have elevated Lp(a) and that no approved treatment for this biomarker, such as statins for elevated LDL, exists.
People do not know if they have elevated Lp(a) because doctors don’t test for it. Doctors do not test for it because it doesn’t result in profit for them since they can not give you a drug.
But now, with this drug in phase II drug trials, expect to see more doctors testing your Lp(a) levels, letting you know a pill is on the way to save you.
I cannot see the complete Phase II study, just the abstract. The 12-week study was conducted on 233 adults, with 67 participants in the placebo group. The abstract does not indicate if the placebo was a sugar pill or another drug.
I wonder about the placebo in the study because the article states that adverse events were similar in both groups. We would assume that the placebo is a sugar pill. However, since the control group rarely receives a saline placebo in vaccine trials, could the placebo group in these trials be another drug? It would be nice if this were clarified.
The study results found no change in the hs-CRP biomarker. (To learn more about the hs-CRP biomarker and its importance, read this substack).
The researchers admit that much more extensive studies are required to determine if lowering Lp(a) has any benefits, such as reducing the risk of a cardiovascular event.
Determining if the drug prevents cardiovascular events in people with elevated Lp(a) is critical. In statin trials, they only had to show that the drug reduced total and LDL cholesterol; they did not have to show that it prevented a cardiovascular event.
Research indicates that the more you lower your LDL, the greater your risk of heart attacks and strokes, all the while causing joint pain, severe fatigue, and dementia.
The full text of the phase I trials is available. During phase I, the doses used were broader, up to 800 mg. In phase II, the dose only went as high as 240 mg per day.
In the 14-day trial, 62% reported 71 adverse events in the single ascending dose group, and 80% reported 175 adverse events in the multiple ascending dose group. The investigator considered the adverse events mild, such as headache, fatigue, and abdominal pain.
What are the adverse events in the 12-week study? If anyone has access to the full text of the phase II trial, please share!
Bottom Line: Once this drug is approved, expect to see the Lp(a) biomarker in your labs. If it is elevated, prepare for your medical professional's pharmaceutical speech.
What will you do if you find out you have a genetic risk factor for cardiovascular disease?
Show my posts some love, please!
It is just me writing, reading, researching, and seeing clients!
I do not use mainstream social media, so please share my posts so that more people can get informed on how to get and stay healthy.
This is NOT information allopathic practitioners will share with you.





I know of an entire family (all grown and with their own kids now) who was repeatedly getting skin cancers. They all started taking niacin and solved it!
What's the current lag time between being considered a conspiracy theory and being accepted as factual? I know it keeps getting shorter all the time.